No discussion of gut health and methylation would be complete without considering the problem of oxalates. I understand many of you reading this may not have heard of oxalates before. However, just because you haven’t heard of them doesn’t mean they aren’t a potential problem! Like many things in life moderation is the key; our body has the ability to manage mild levels of oxalates. But if oxalate levels build up too high we are certain to suffer consequences in our health and our genetic pathways. So let us investigate why oxalates rise inside our bodies and how they cause us harm.
While there are some rare, genetic causes for having high oxalates, the vast majority of people with oxalate problems cannot blame it on their genes. As you will soon learn, the main reason oxalates become a problem is that they leak in through a dysfuctional gut. Since most Americans have a leaky gut of some kind, more and more people are developing oxalate-related issues. And the worst part is that those who have an oxalate problem likely have no idea. Oxalates aren’t something most doctors are aware of and we don’t hear much about them in the media or casual conversations. But if you ask a person who has just had to deal with a painful kidney stone, they will tell you just how big of a problem oxalates can be!
SNPs of Concern
As we dive into the topic of oxalates there are certain SNPs that are important to keep in mind. But before I talk about these polymorphisms I want to remind you of something you will hear again and again throughout this book; that is our genes are not our destiny, but they are our tendency. This idea is critical to understand because the environment inside the body truly does rule the roost. In other words as we talk about oxalate issues and low sulfate problems we are really talking about an environmental issue inside the body. And lucky for us we can change the environment and help our genes express their best – we have the power to optimize our genes by changing the environment! For more info on how to heal oxalate issues then please refer to the Oxalate Protocol.
What you are about to discover is that oxalates create biochemical problems that make methylation issues worse. Since oxalate problems cause sulfate problems, the genes most effected will be the SULT and other phase II related pathways. The sulfate molecule is key in order for the liver to perform the daily task of detoxification. If sulfate levels drop, then the body cannot use the SULT pathway to detoxify. Instead it will be forced to use other Phase II pathways which can put greater demand on pathways that are also genetically slowed down. When we consider other slowed Phase II detoxification gene SNPs such as NAT2, ALDH, COMT, GSH, GSS, UGT, and SOUX we can begin to see that a lack of sulfate molecules can have a broad negative impact on all of our detoxification pathways.
Even without an oxalate issue people with SULT SNPs have slowed detoxification and are going to be sensitive to toxins, hormones, xenobiotics, and heavy metals. Additionally, individuals who have SULT SNPs will be extra sensitive to low sulfate levels, since lack of sulfate will exacerbate a slowed genetic pathway. Many people with SULT gene polymorphisms will also be sensitive to food colorings and additives in processed foods since these chemicals are phenols which slow down SULT pathways even more. Without knowing it people are literally clogging their SULT pathway with toxins, oxalates, food colorings and more.
When we realize that oxalate problems create low sulfate issues, it becomes clear that individuals with MTHFR and related gene SNPs will also suffer (the topic of sulfates and oxalates will be thoroughly covered in a post). Remember that MTHFR and methylation cycle pathways help the body to grow, repair, and detoxify all sorts of compounds. As you will soon see, when oxalate levels are high, sulfate levels drop slowing down detoxification. Low sulfate levels put extra stress into the methylation cycle to provide the body with sulfate molecules. In individuals with an impaired methylation cycle this can provoke methylation issues such as high homocysteine, developmental disorders, gallbladder dysfunction, hormone imbalances, excess inflammation, poor growth and to name but a few. So with oxalate issues and the biochemical chaos it creates, a great deal of stress is placed on the methylation cycle.
Oxalates and Leaky Gut
As I mentioned in the introduction poor digestion is the main reason people develop oxalate problems. And without a doubt a poor functioning gallbladder is the number one reason we develop oxalate problems. To illustrate the connection between gut dysfunction and oxalates, we start by looking at how oxalate levels rise after bariatric surgery. Research has shown that individuals who compromise their upper GI tract with Roux-En-Y bypass surgery develop hyperoxaluria – excess oxalates in the blood and urine.1 This bariatric surgery oxalate relationship is very easy to understand. When we damage the stomach and gallbladder with an aggressive surgery, it begins to impair digestion. And as digestion becomes more dysfunctional, more oxalate problems develop. Simple as that.
Oxalates are found in many common foods such as caffeine, chocolate, nuts and seeds, and many varieties of fruits and vegetables (a list of low oxalate foods is provided on the Oxalate Protocol page).2 Oxalates are also found in the connective tissue of animals so human omnivorous eating animal protein at meals will undoubtedly be consuming some oxalates as well.3 When we eat our kale salads or drink our spinach smoothies we are getting the nutrients and antioxidants in those plants; but we are also getting the oxalates. Most people don’t realize that by juicing every day that they may be overdosing on oxalates. But don’t despair and think I am saying that these foods are bad for you.
Foods that contain oxalates are some of the healthiest foods we can eat – spinach, blueberries, kale, etc. As long as our digestion is working properly, producing stomach acid and releasing enzymes and bile, the oxalates in food are not a problem. As long as our gallbladder is working well, we can eat food with oxalates and have no worries that we will develop an oxalate problem. The problem with oxalates arises because we don’t exactly have healthy gallbladders in this country.
As I showed in the last chapter, digestion should stimulate the release of bile from the gall bladder allowing us to digest fats in our diet. The problem is that many people suffer from terrible gallbladder function, and gallbladder surgery is still one of the most common surgeries in America.4 It’s the bile from the gallbladder that helps us fend off the negative effects of oxalates. Without bile release from a healthy gallbladder, oxalates are going to become a problem, esp. for those with chronic gut or methylation problems.
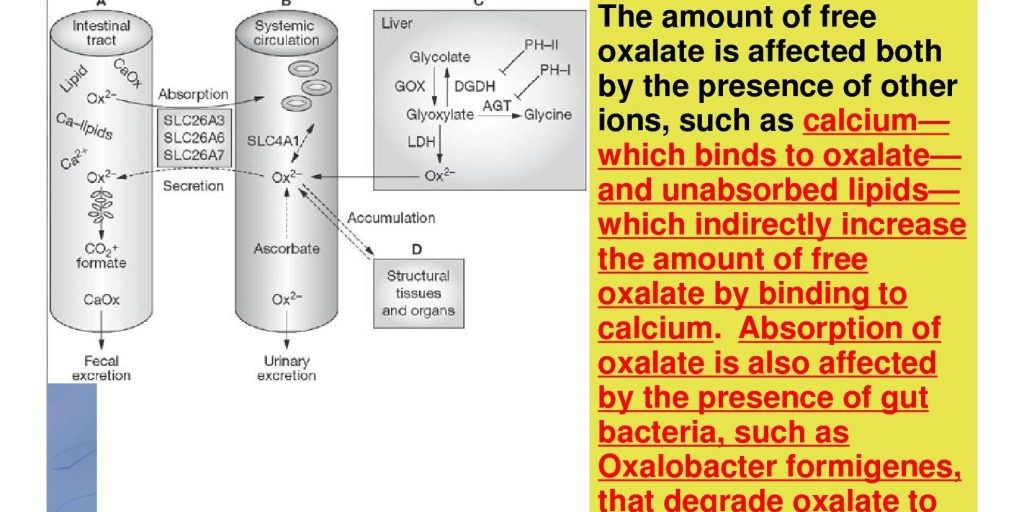
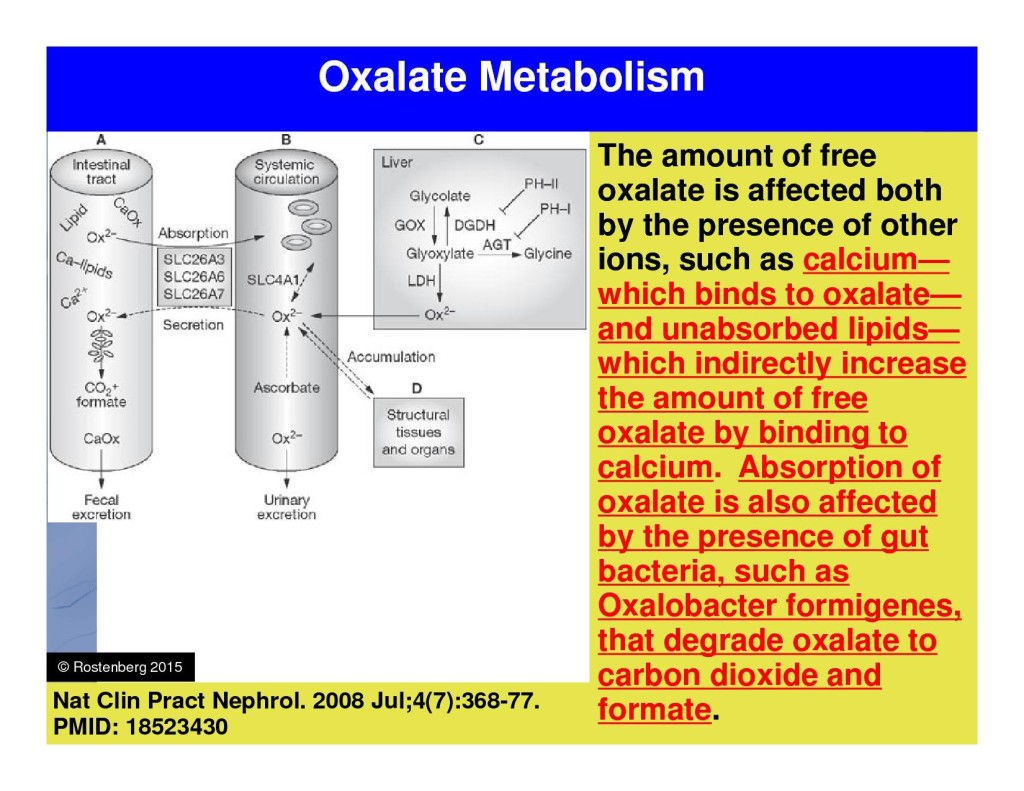 Figure 4.1 – Pathways and mechanisms of how oxalates are absorbed and produced inside the human body.
Figure 4.1 – Pathways and mechanisms of how oxalates are absorbed and produced inside the human body.
Bile acts like soap and soap chops fat globules into tiny balls called micelles – a chemical property we need in order to absorb all those healthy Omega 3 fats and fat-soluble vitamins like A, D, E, and K. When the gallbladder is working properly the fat in our diet is absorbed in the small intestine and the oxalates in our meal form a compound with calcium called calcium-oxalate which we cannot absorb.5 In this way bile helps us absorb the fats we need and pass the oxalates in the stool so they don’t cause problems (Figure 4.1). Normally our body will not absorb all calcium from out diet. The undigested calcium is needed to bind with the oxalates in the gut which helps us to rid our body of this toxic molecule. However the same cannot be said when the gallbladder system begins to malfunction.
When we stop releasing bile, whether it is from stomach dysfunction, taurine deficiency, or some other health problem (like having the gallbladder removed surgically), we will start to absorb more oxalates.6 This occurs because without bile release we cannot absorb fats. Since the fats are floating down the small intestine without being absorbed, they begin to bind with all the calcium. Remember when I said that calcium is required to bind with the oxalate in order to neutralize it? Well when the fat isn’t digested then the calcium gets attached to the fats instead of the oxalate. This causes us to poop out all our healthy fats and our calcium, leading to significant nutritional and health problems down the road like osteoporosis and inflammatory diseases. When we do not absorb fats properly there is no calcium left to bind to the oxalates, and we end up absorbing high amounts of oxalates. As you will see, this will cause problems in other parts of our body.
Calcium and Kidney Problems
One of the big problems with oxalates is that they cause imbalances in the kidneys, bones and liver. The kidneys are especially sensitive to oxalates, where they have a tendency to cause kidney stones. I have personally never suffered with a kidney stone, but based on the experiences reported to me by my patients it sounds absolutely terrible! And not surprisingly the latest research on kidney stones points clearly to problems in the gut as the root cause. Taking a closer look at the biochemical research we can see clearly how oxalates, and by extension gut problems, are the most common cause of kidney stone suffering.
From research published in the New England Journal of Medicine going back forty years, we have the first indications that gut problems can cause oxalate issues in the kidney. Researchers investigating ulcerative colitis patients found that after sections of the ileum had been surgically removed that many individuals developed hyperoxaluria, a known risk factor for stone formation.7 A later study published in 2010 highlighted the fact that almost 75% of all kidney stones are in fact calcium-oxalate stones, further cementing the connection between kidney damage and oxalate levels.6 What both these studies confirm is that most people in the USA who have a kidney stone are actually suffering from an oxalate problem that starts in the gut!
In a more recent study released in 2015 researchers confirmed that not only do oxalates cause most kidney stones, they also play a role in robbing the body of calcium leading to bone degeneration and osteoporosis.8 This illustrates that we don’t just suffer oxalate problems in the gut and the kidney, they have effects on our bones as well! When the gut cannot provide an adequate level of calcium for the rest of the body, the bones are broken down to release calcium into the bloodstream. If this happens long enough, bone loss and osteoporosis is the result. Too bad no one tells you that when you get your gallbladder removed!
Many readers have probably heard someone say that “excess” calcium can give you kidney stones. But we cannot blame calcium when the problem is caused by oxalates. Oxalates hurt the kidney and other tissues because they are one of the most insoluble compounds in the body.9 This means if levels rise too high then oxalates will form crystals and will be almost impossible for the body to dissolve. They can deposit in the brain, lungs, blood vessels, joints and bones causing pain and dysfunction throughout our body.10-13 Forming oxalate crystals inside the body can be a hidden source of pain and dysfunction in dozens of chronic health problems ranging from autism to fibromyalgia to vulvodynia and more. Geez and you thought eating spinach, kale and chard smoothies every day could do no harm!
At this point I have one more important question to ask: If calcium-oxalate stones are what cause most kidney stones, should you avoid calcium in your diet? Well, what do you think? Now this question is tricky so I am going to help you out – the answer is No! More calcium, not less, will be needed in your diet if you want to prevent oxalate stones from forming. While this sounds completely contradictory, the body has a genius reason for why it does this. Research has proven that eating more calcium in the diet will actually prevent calcium-oxalate stones by binding up more of the oxalates in your gut.14 This apparent paradox is solved by remembering that oxalate kidney stones are really just a gut problem that shows up as a problem the kidney. In other words when you fix the gut, you fix the kidney’s oxalate problem.
When faced with the problem of oxalates leaking into the gut, one of the best strategies is to take calcium-citrate with meals. This type of calcium does two things. First, calcium-citrate releases its calcium quickly into the gut, helping to bind up the extra oxalates floating around. And second the citrate helps to prevent the calcium and the oxalate from binding inside the kidney.15, 16 That’s a 2 for 1 that pays off! I routinely recommend this to my patients with excellent results. More specific information on how to heal oxalate problems with diet and supplements can be found here.
I wish I could stop here and say that is all the damage that oxalates can do to our body, but that would fall short of capturing the full story. In addition to robbing us of calcium, healthy fats and fat-soluble vitamins, and causing kidney stones, oxalates also deplete us of sulfate and vitamin B6. These two vitamins are incredibly powerful and are absolutely necessary for our health and survival. But the rest of this important story will have to wait. Stay tuned for future posts where I will give you even more important information about oxalate toxicity and methylation problems.
Diet and Supplement Recommendations
Now that you have some idea of the toxicity of oxalates its time to look at how to fix the issue. I will share with you some helpful concepts for protecting your body from the toxic burden of oxalates. The good news is that treating oxalate problems is fairly simple. You will find the dietary advice and supplement recommendations I use with patients under the protocols section.
In Health,
Dr. Rostenberg
By studying the current peer-reviewed research, Dr. Rostenberg has discovered powerful, natural strategies to optimize gut and methylation function to heal the body. He can help you uncover the genetic or root causes of your health problem and find a natural solution! If you would like help balancing your oxalate levels to improve your methylation cycle and reduce/eliminate your symptoms, please contact Dr. Rostenberg at Red Mountain Natural Medicine today. Phone 208-322-7755. Email redmountainclinic@gmail.com. Website https://www.redmountainclinic.com
REFERENCES
- Kumar R, Lieske JC, Collazo-Clavell ML, et al. Fat malabsorption and increased intestinal oxalate absorption are common after Roux-en-Y gastric bypass surgery. Surgery. 2011 May;149(5):654-61.
- Low Oxalate Diet May Help Prevent Kidney Stones. University of Pittsburg Medical Center Web Site. http://www.upmc.com/patients-visitors/education/nutrition/pages/low-oxalate-diet.aspx. Accessed on 10/17/2015.
- Nguyen QV, Kälin A, Drouve U, et al. Sensitivity to meat protein intake and hyperoxaluria in idiopathic calcium stone formers. Kidney Int. 2001 Jun;59(6):2273-81.
- Common Surgical Procedures. The University of Chicago Medicine web site. http://www.uchospitals.edu/online-library/content=P01392. Accessed on November 27, 2015.
- Marengo SR, Romani AM. Oxalate in renal stone disease: the terminal metabolite that just won’t go away. Nat Clin Pract Nephrol. 2008 Jul;4(7):368-77.
- Evan AP. Physiopathology and etiology of stone formation in the kidney and the urinary tract. Pediatr Nephrol. 2010 May; 25(5): 831–841.
- Dobbins JW, Binder HJ. Importance of the colon in enteric hyperoxaluria. N Engl J Med. 1977 Feb 10;296(6):298-301.
- Yiu AJ, Callaghan D, Sultana R, et al. Vascular Calcification and Stone Disease: A New Look towards the Mechanism. J Cardiovasc Dev Dis. 2015;2(3):141-164.
- Shaw, W. Oxalates Control is a Major New Factor in Autism Therapy. Great Plains Laboratory. http://www.greatplainslaboratory.com/home/eng/oxalates.asp. Accessed on November 27, 2015.
- Ghio AJ, Roggli VL, Kennedy TP, et al. Calcium oxalate and iron accumulation in sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2000 Jun;17(2):140-50.
- Ott SM, Andress DL, Sherrard DJ. Bone oxalate in a long-term hemodialysis patient who ingested high doses of vitamin C. Am J Kidney Dis. 1986 Dec;8(6):450-4.
- Hall BM, Walsh JC, Horvath JS, et al. Peripheral neuropathy complicating primary hyperoxaluria. J Neurol Sci. 1976 Oct;29(2-4):343-9.
- Sahin G, Acikalin MF, Yalcin AU. Erythropoietin resistance as a result of oxalosis in bone marrow. Clin Nephrol. 2005 May;63(5):402-4.
- Hess B, Jost C, Zipperle L, et al. High-calcium intake abolishes hyperoxaluria and reduces urinary crystallization during a 20-fold normal oxalate load in humans. Nephrol Dial Transplant. 1998 Sep;13(9):2241-7.
- Berg, C. Alkaline citrate in prevention of recurrent calcium oxalate stones. Scand J Urol Nephrol Suppl. 1990;130:1-83.
- Ohana E, Shcheynikov N, Moe OW, et al. SLC26A6 and NaDC-1 transporters interact to regulate oxalate and citrate homeostasis. J Am Soc Nephrol. 2013 Oct; 24(10): 1617–1626.